Navigating Your Medications: A Comprehensive Guide to Adverse Effects, Contraindications, and Drug Interactions
Medications are powerful tools in managing our health, offering relief, healing, and even life-saving interventions. Yet, their very potency means they come with complexities. Taking a drug isn't just about swallowing a pill; it's about introducing a chemical agent into a dynamic biological system, one that's constantly interacting with everything else we consume and every condition we live with. Understanding Adverse Effects, Contraindications, and Drug Interactions isn't just medical jargon; it's vital knowledge for anyone hoping to use their prescriptions and over-the-counter remedies safely and effectively.
It's about being an informed participant in your own healthcare, recognizing the subtle signals your body sends, and asking the right questions. Whether you're managing a chronic condition, taking a short course of antibiotics, or simply reaching for a pain reliever, being aware of these potential pitfalls can make all the difference between a beneficial outcome and a serious health setback.
At a glance: Your safety checklist for medications
- Your body is unique: How a drug affects you can be different from anyone else due to genetics, diet, other medications, and existing health conditions.
- Knowledge is power: Understand what your medication is for, how to take it, and what to watch out for.
- Communication is key: Always tell your doctor and pharmacist about all medications, supplements, and even foods you regularly consume.
- Stay organized: Keep an up-to-date list of everything you take and follow dosage instructions precisely.
- Don't self-diagnose or self-medicate: When in doubt, always consult a healthcare professional.
Decoding the Language of Medication Safety
Before we dive into the intricacies of how drugs interact, let's establish a clear understanding of the core concepts that define medication safety:
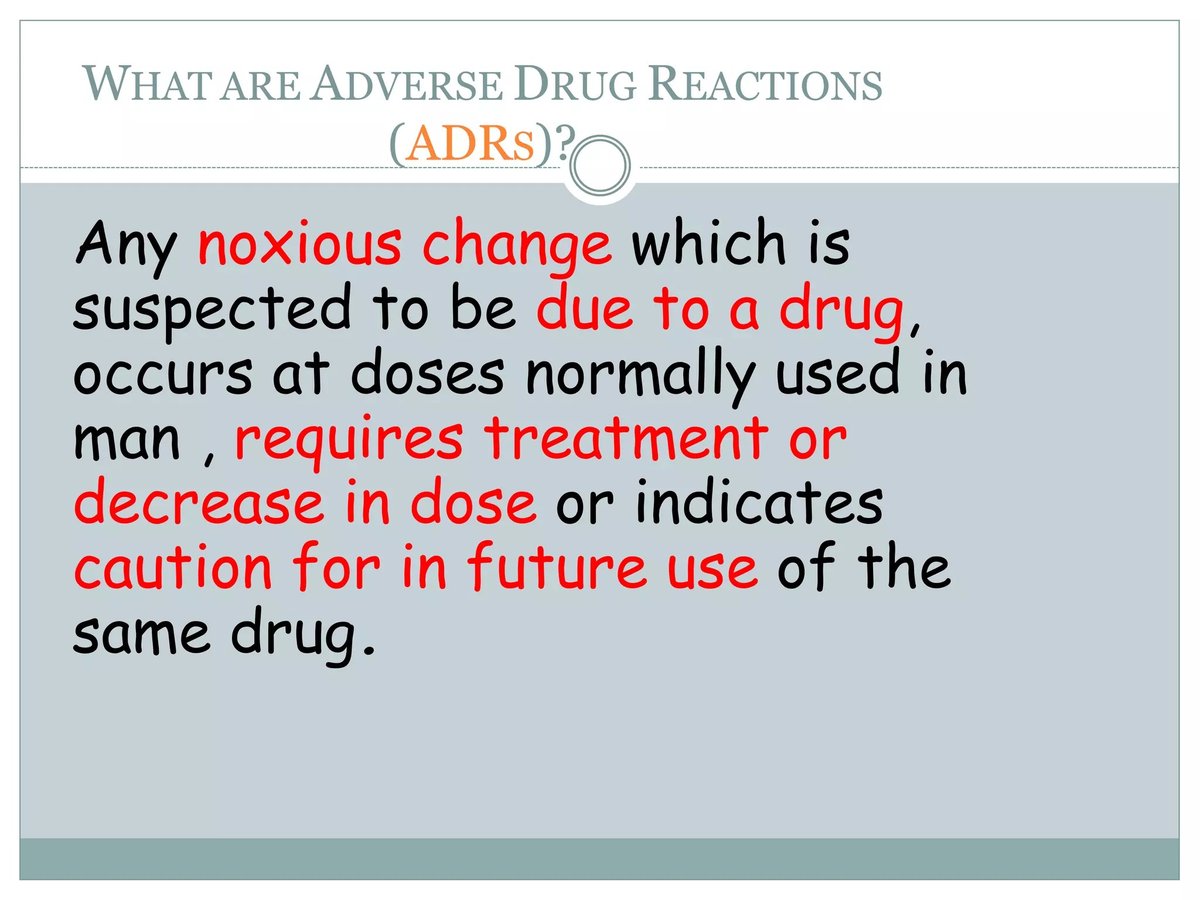
What Are Adverse Effects?
Think of adverse effects as the unwanted guests at your body's party. These are any unintended and undesirable effects of a drug that occur at normal doses. They can range from mild annoyances like drowsiness or a slight stomach upset to severe, life-threatening reactions.
- Predictable vs. Unpredictable: Some adverse effects are predictable based on the drug's mechanism of action (e.g., antihistamines causing drowsiness). Others are idiosyncratic, meaning they occur rarely and unpredictably in certain individuals.
- Dose-related vs. Non-dose-related: Many adverse effects are more likely or severe with higher doses, while others can occur even at therapeutic doses.
- Allergic Reactions: A specific type of adverse effect where your immune system overreacts to a drug. This can manifest as a rash, hives, swelling, or even anaphylaxis, a severe, life-threatening reaction.
It’s crucial to distinguish between a minor side effect you can manage and an adverse effect that warrants medical attention. When in doubt, contact your healthcare provider.
What Are Contraindications?
A contraindication is a specific situation, condition, or factor that makes a particular treatment or procedure inadvisable because it could harm the patient. It's essentially a red flag, signaling that a certain drug should not be used.
- Absolute Contraindications: These mean the drug should never be used. For example, if you have a known severe allergy to penicillin, then penicillin is absolutely contraindicated for you.
- Relative Contraindications: These mean the drug should generally be avoided, but might be used if the benefits clearly outweigh the risks, and with careful monitoring. For instance, a drug might be relatively contraindicated in patients with kidney impairment, meaning the dose might need to be adjusted or an alternative considered.
Contraindications often relate to pre-existing medical conditions (like heart disease or pregnancy), concurrent use of other medications (leading to a dangerous interaction), or specific patient characteristics (like age). Your doctor uses your full medical history to check for these critical warnings.
The Interwoven Web: Understanding Drug Interactions
The term "drug interaction" refers to what happens when two or more substances, taken together, change how one or more of them work in the body. This isn't always a negative outcome; sometimes, interactions are intentionally used to enhance a drug's effect. More often, however, they can reduce a medication's effectiveness, increase its action to dangerous levels, or cause unexpected side effects or toxicity.
These interactions can be temporary and manageable, but it’s vital to recognize that they can also escalate to serious or even fatal consequences. Understanding the various pathways through which drugs and other substances interact is your first line of defense.
Substances that can trigger these complex chemical dances include a wide array of everyday items:
- Other medications, both prescription and over-the-counter (OTC)
- Dietary supplements, including vitamins, minerals, and herbal remedies
- Specific foods or beverages
- Alcohol, tobacco, and recreational drugs
While anyone can experience a drug interaction, your risk increases significantly if you're taking multiple medications, managing several health conditions, or as you get older, due to changes in how your body processes drugs.
1. Drug-Drug Interactions: When Medications Clash
This is perhaps the most commonly recognized type of interaction, where one medication directly alters how another works in your body. This can happen between two prescription drugs, two OTC drugs, or a combination of both. Even substances like tobacco, alcohol, or recreational drugs can act as "drugs" in this context, instigating interactions.
- Worsened Side Effects: Imagine taking two different medications, both of which list drowsiness as a potential side effect. Taken together, this effect could be dramatically amplified, making it unsafe to drive or operate machinery. A common example involves accidentally taking two different OTC products (e.g., a cold medicine and a pain reliever) that both contain acetaminophen, leading to a dangerous overdose risk.
- Reduced Effectiveness: Some drugs have antagonistic actions, meaning they essentially cancel each other out. A classic example is when certain antibiotics can reduce the effectiveness of oral contraceptives, requiring alternative birth control methods.
- Altered Metabolism or Absorption: Many interactions occur in the liver or gut. One drug might speed up the liver's breakdown of another drug, making it less potent and less effective. Conversely, a drug might slow down the breakdown of another, causing it to build up to toxic levels in the body. For example, some antibiotics can increase the blood-thinning effect of warfarin by affecting its metabolism.
2. Drug-Supplement Interactions: Natural Doesn't Always Mean Safe
Dietary supplements—vitamins, minerals, and especially herbal remedies—are often perceived as benign because they're "natural." However, many contain potent bioactive compounds that can interact just as powerfully with prescription medications as other drugs do. These interactions can make medications less effective, dangerously potent, or lead to serious side effects.
- St. John's Wort: This popular herbal remedy for depression is a notorious interactant. It can significantly reduce the effectiveness of many drugs, including antidepressants (potentially leading to a dangerous condition called serotonin syndrome if taken with SSRIs), birth control pills, certain heart medications, and antiretrovirals.
- Garlic Extracts: Known for their blood-thinning properties, concentrated garlic supplements can heighten the risk of bleeding when taken with anticoagulant medications like warfarin or before surgery.
- Goldenseal: This herb can interfere with the liver's processing of many drugs, potentially leading to increased drug levels and toxicity.
- Concentrated Green Tea Supplements: While green tea itself is generally safe, highly concentrated supplements might interact with certain medications like pseudoephedrine, a decongestant.
High Risk Scenarios: Individuals taking medications with a narrow therapeutic range are at particularly high risk. These are drugs where the difference between a therapeutic dose and a toxic dose is very small (e.g., carbamazepine, phenytoin, cyclosporine, digoxin, warfarin). Even slight changes in their blood levels due to an interaction can have dangerous consequences. It's also critical to disclose all supplements before any surgery, as they can affect anesthesia, blood clotting, blood pressure, or heart rate.
3. Drug-Food/Beverage Interactions: Your Plate and Your Pill
What you eat and drink can significantly impact how your body processes medication. Certain foods and beverages can prevent proper absorption, change how a drug moves through your system, alter its metabolism (making it more or less effective), or prevent its elimination, potentially leading to toxicity.
- Vitamin K and Warfarin: Foods rich in Vitamin K, such as leafy green vegetables (spinach, kale, broccoli), can reduce the effectiveness of warfarin, a blood thinner. Maintaining a consistent intake of Vitamin K is important, rather than avoiding it entirely, to ensure stable warfarin levels.
- Grapefruit (and Grapefruit Juice): A potent example, grapefruit can interact with over 85 different medications. It inhibits an enzyme in your gut that normally breaks down certain drugs, leading to much higher levels of the drug in your bloodstream. This can be dangerous for medications like some statins (e.g., simvastatin, atorvastatin), certain blood pressure drugs, and organ-transplant medications. The effect can last for days after consuming grapefruit.
- Dairy Products: Calcium in dairy products (milk, yogurt, cheese) can bind with certain medications like levothyroxine (for thyroid), bisphosphonates (for osteoporosis), and some antibiotics (like tetracyclines and fluoroquinolones), preventing their absorption. These drugs often need to be taken hours apart from dairy.
- Tyramine-Rich Foods: Aged cheeses, cured meats, fermented products (sauerkraut, soy sauce), and some alcoholic beverages contain tyramine. When consumed by individuals taking certain antidepressants called MAOIs (Monoamine Oxidase Inhibitors), or other drugs like linezolid or isoniazid, it can lead to a dangerous surge in blood pressure (hypertensive crisis).
- Alcohol: Alcohol is a drug in itself, and its interactions with medications are numerous and often serious. It can increase drowsiness with sedatives, lead to severe nausea and vomiting with metronidazole, increase the risk of bleeding with warfarin, and significantly heighten liver damage risk when combined with acetaminophen. Even drugs like oral third-generation cephalosporin can have specific interactions that affect absorption or metabolism, impacting their efficacy.
- Timing is Everything: Some drugs require an empty stomach for optimal absorption, while others must be taken with food (or even specific types of food, like high-fat meals) to work properly or reduce stomach upset. Always clarify these instructions.
4. Drug-Condition Interactions: When Your Health Profile Shifts the Balance
Sometimes, a medication prescribed to treat one health issue can worsen another existing medical condition or trigger unwanted effects because of your underlying health status. This isn't about two external substances clashing, but rather how a drug interacts with your body's specific physiological state.
- Hypertension Risk: Many common medications can elevate blood pressure. Nasal decongestants (like pseudoephedrine), amphetamines, NSAIDs (Nonsteroidal Anti-Inflammatory Drugs like ibuprofen), and even some steroids can raise blood pressure, posing a significant risk for individuals already living with hypertension.
- Increased Risk Conditions: Certain pre-existing conditions make you more susceptible to drug-condition interactions:
- Bladder Control Issues: Some medications can worsen urinary retention.
- Diabetes: Certain drugs can affect blood sugar levels, requiring careful monitoring.
- Enlarged Prostate: Some drugs can exacerbate symptoms.
- Glaucoma: Certain medications can increase eye pressure.
- High or Low Blood Pressure: Drugs that affect the cardiovascular system need careful consideration.
- Insomnia: Stimulant drugs or even some antidepressants can worsen sleep problems.
- Stomach Ulcer: NSAIDs are well-known for increasing the risk of ulcers and bleeding.
It's critical that your healthcare provider has a complete and accurate picture of your medical history, including all past and present diagnoses, to prescribe medications safely.
Your Shield Against Interactions: Preventing Problems Proactively
The good news is that most adverse effects, contraindications, and drug interactions are preventable. Your active participation in your healthcare, combined with diligence and clear communication, forms the most effective defense.
1. Maintain an Updated, Comprehensive Medication List
This is arguably the most crucial step. Think of it as your medication passport. Keep an active, detailed list of everything you take, and update it immediately with any changes.
What to include:
- Full name of each drug/supplement: (e.g., "Aspirin," not just "blood thinner").
- Active ingredients: Especially for OTC products, as different brands may contain the same active ingredients.
- Reason for taking: (e.g., "for blood pressure," "for headaches").
- Dose: (e.g., "20 mg").
- Frequency: (e.g., "once daily," "every 4-6 hours").
- Duration: (e.g., "for 10 days," "long-term").
- Special instructions: (e.g., "take with food," "avoid dairy").
- Prescribing doctor: If applicable.
Actionable Tips: - Share with everyone: Provide a copy to every healthcare provider you see (doctors, specialists, dentists, nurses) and your pharmacist.
- Use one pharmacy: Sticking to a single pharmacy allows their system to track all your prescriptions and flag potential interactions automatically.
- Keep copies handy: Keep a copy at home, a digital version on your phone, and a printed copy in your wallet or purse, especially when traveling. This is invaluable in emergencies.
2. Communicate, Communicate, Communicate with Healthcare Providers
Never assume your doctor or pharmacist knows everything you're taking or that a "minor" supplement isn't important. Full disclosure is non-negotiable for your safety.
When to talk to your doctor or pharmacist:
- Before taking any new drug or supplement: This includes OTC medications, vitamins, herbs, or even remedies you've used safely in the past. Your current medication regimen might have changed.
- Before making any changes: Never stop taking a prescribed medication or alter its dose without consulting your doctor.
- If you have questions: Don't hesitate if you don't understand instructions, miss a dose, develop new side effects, or feel a medication isn't working as it should.
- When prescribed a new drug: This is your prime opportunity to discuss everything else you consume:
- All prescription drugs
- All over-the-counter drugs (pain relievers, antacids, cold remedies)
- Dietary supplements (vitamins, botanicals, minerals, herbals)
- Alcohol intake
- Tobacco use
- Recreational drugs
- Any unusual or concentrated food consumption (e.g., daily grapefruit juice).
Key Questions to Ask (and expect answers to): - "How much of this medication should I take, and how often?"
- "Should I take it with food or on an empty stomach?"
- "Are there any specific foods or drinks I should avoid while taking this?"
- "Are there other medications or supplements I need to stop taking or avoid while on this?"
- "What are the most common side effects, and when should I call you?"
- "How will I know if this medication is working?"
For prescription drugs, always ask your pharmacist for the detailed package insert. While dense, it contains comprehensive information about interactions, contraindications, and adverse effects.
3. Stay Organized and Establish Routines
Consistency and organization can prevent many simple but dangerous errors.
- Use a calendar or planner: Mark medication schedules to ensure you take doses correctly and on time.
- Utilize a pill box/organizer: These are excellent for tracking daily or weekly doses, reducing the chance of missed or double doses. Just be sure to keep it out of reach of children and pets.
- Set reminders: Phone alerts, smart speaker reminders, or even sticky notes can be invaluable cues.
- Inform a household member: If you live with others, let them know your medication schedule and where your list is stored, especially important if you live alone or have complex medical needs.
Empowering Yourself with Information: Using Resources Wisely
In the age of information, resources are abundant, but discernment is key.
Reading Over-the-Counter (OTC) Drug Labels
Don't skip the small print on OTC labels! These labels are a treasure trove of vital safety information. Always pay close attention to:
- "Active Ingredients": This tells you the specific chemical working in the drug. Many different brands of cold medicine, for instance, might contain the same active ingredients (e.g., acetaminophen or ibuprofen). Taking multiple products with the same active ingredient concurrently can lead to an accidental overdose.
- "Warnings": This section explicitly lists potential adverse effects, contraindications, and common drug interactions (e.g., "Do not take with other products containing X," or "Ask a doctor before use if you have Y condition").
- "Directions": Precisely follow dosage instructions and frequency. More is not better, and less might be ineffective.
Always be aware that OTC labels can change, so a quick read-through before each purchase is a good habit.
Online Drug Interaction Checkers vs. Professional Advice
Online drug interaction checkers and charts can be helpful screening tools, offering quick insights into potential interactions between drugs, or drugs and foods. They are valuable for prompting questions and increasing awareness.
However, they are not a substitute for professional medical advice.
- Limited Scope: Online tools often don't account for your unique medical history, specific health conditions, genetic factors, or the severity of potential interactions.
- Generalized Information: They may not have the most up-to-date information for every possible interaction or nuanced clinical considerations.
- No Personalized Context: A healthcare provider can weigh the risks and benefits in the context of your overall health, other treatments, and lifestyle, offering personalized guidance.
Your doctor and pharmacist are your primary, most reliable sources for up-to-date, personalized guidance on drug interactions and medication safety. They have access to comprehensive databases and, more importantly, your complete medical profile.
Special Considerations
- Pregnancy and Breastfeeding: These are critical times when almost any medication or supplement can affect the baby. Always consult your doctor before taking anything.
- Allergies: If you're prone to allergic reactions, always wear a medical alert bracelet and clearly communicate all known allergies to your healthcare providers.
Moving Forward with Confidence and Caution
Understanding Adverse Effects, Contraindications, and Drug Interactions might seem like a daunting task, but it doesn't have to be. By adopting a proactive mindset and making communication a cornerstone of your healthcare interactions, you transform from a passive recipient of medicine to an informed manager of your health.
Your medications are there to help you, but their power demands respect and vigilance. Keep your lists updated, ask every question that comes to mind, and never hesitate to seek professional guidance. In doing so, you're not just taking a pill; you're actively safeguarding your well-being, ensuring that every treatment you undertake is as safe and effective as possible. Your health journey is a partnership, and your informed participation is the key to its success.